Symptoms, Cause, Anatomy & Testing
Carpal Tunnel Syndrome (CTS) is considered as themost common entrapment neuropathy (3). The condition is a compressive neuropathy caused by a mechanical distortion produced by compressive forces and compression of the median nerve (2). The pathology is known to be more common in females than males with a 7:3 ratio and known to be more prevalent during the fourth to seventh decades, but can occur in all age groups.
Symptoms & Clinical Features
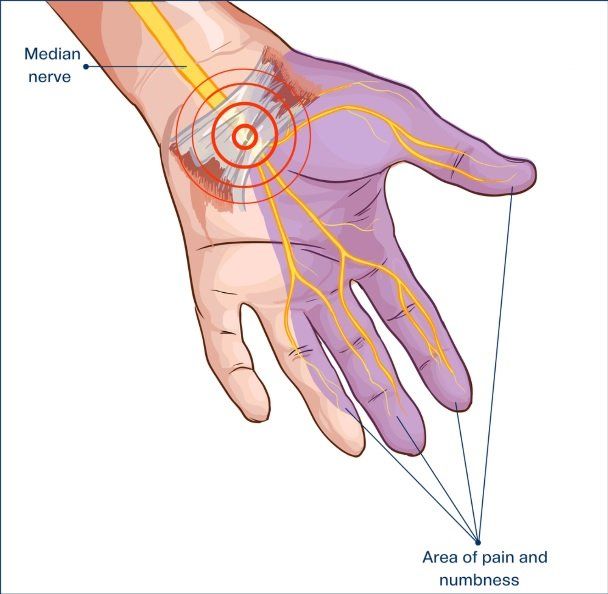
Most patients may complain of aching, tingling, burning or numbness within the hand localised to the first three digits and sensory distribution of the median nerve (3, 5). Symptoms are typically worse in the morning and night and often made worse by strenuous wrist movements which becomes more persistent as the entrapment worsens (3, 5).
A progression of symptoms of CTS involve muscular weakness and atrophy within the thenar eminence and at the base of the thumb. Individuals can often experience an abnormally large increase in carpal tunnel pressure, especially during extreme wrist motions and whilst making a fist (3).
Aetiology & Cause
Activities that often implicate the symptoms in individuals are those who perform and create repetitive movements of the surrounding tendons and thus cause compression of the median nerve within the carpal tunnel.
Such activities may include (3):
- Typing
- Knitting
- Scrubbing
- Dishwashing
- Driving
- Painting
- Gardening
- Lifting
- DIY
Other activities that may irritate the structures are trading industries, especially within the building trade who constantly perform twisting or aggressive jarring movements with their hands or wrists whilst using hammers or drills. Therapists (in all sectors) along with those in office related jobs and regularly use laptops or the mouse. It is also common to see amongst individuals who perform heavy lifting of weights, pushing heavy weights via lifting bars at the gym or difficult objects in warehouses and building sites (3).
Medical Conditions:
Some medical conditions are associated with carpal tunnel syndrome and may include(3):
- Pregnancy
- Lactation
- Menstrual cycles
- Oral contraceptive use
- Menopause
- Diabetes mellitus
- Pyridoxine deficiency
- Toxic shock syndrome
- Chronic haemodialysis
- Osteoarthritis of the carpal bones
- Rheumatoid arthritis
- Obesity
- Amyloidosis
- Mucolipidosis (metabolic disorder)
- Chondromalacia
- Myxoedema (advanced hypothyroidism)
- Acromegaly
- Congenitally small carpal tunnel
- Athetoid dystonic cerebral palsy; a movement disorder caused by damage to the developing brain.
Anatomy
The boundaries of the carpal tunnel consist of the carpal bones which form the floor (Trapezium, Trapezoid, Capitate, Hamate); and the flexor retinaculumwhich is situated between the transverse carpal ligament (CL) (also known as the flexor retinaculum) which is positioned superiorly along with nine flexor tendons; flexor digitorum superficialis, flexor digitorum profundus (x 5) (3, 5). The flexor pollicis longus tendons also pass through the carpal tunnel. The carpal bones; the scaphoid and trapezium are positioned inferiorly. The tendons are surrounded by synovial sheaths which is designed to reduce friction between the structures (3).
Within the tunnel, the median nerve divides into a muscular branch to supply the thenar eminence and palmer digital branch to supply sensation of the palmer aspect of the lateral three and half digits and lateral two lumbricals.
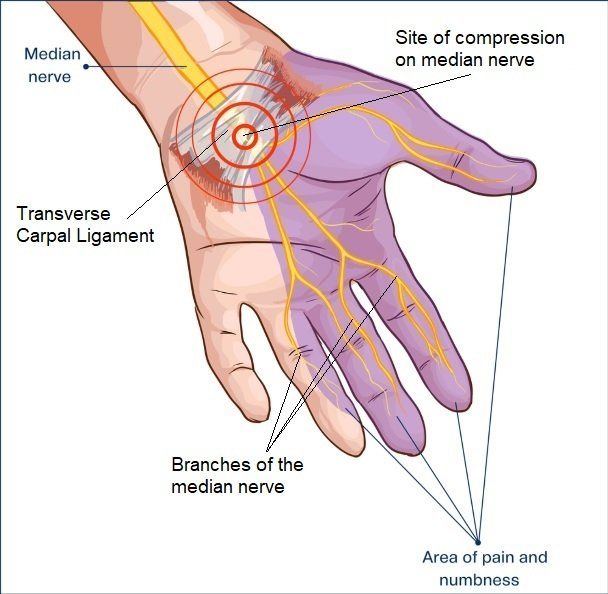
Figure 2: Sight of compression of the median nerve within the carpal tunnel
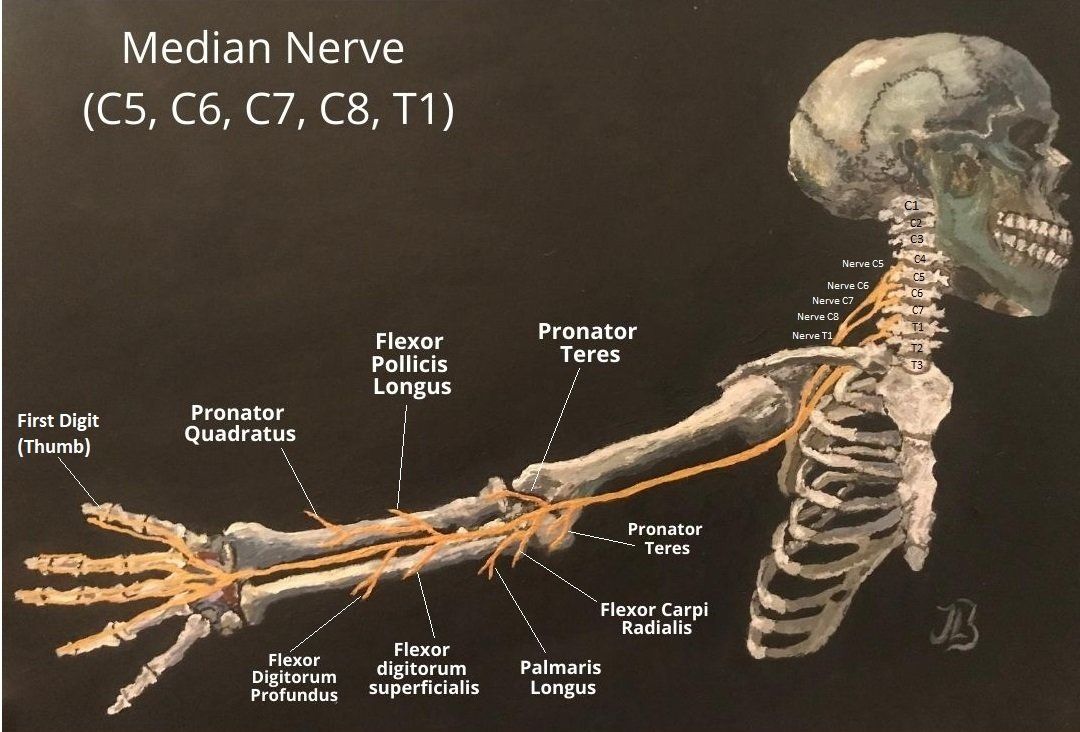
Course of the Median Nerve
The median nerve originates from the lateral and medial cords of the brachial plexus and has contributions from ventral cervical nerve roots C5 to C7 (lateral cord) and C8 and T1 (medial cord) (3, 8). McNamara (2003) interestingly reports that the nerve only sometimes receives fibres from C5 and mainly originates from C6-T1 nerve fibres.
The median nerve is formed from the medial and lateral cords of the brachial plexus as the nerves merge within the axilla (6). The median nerve continues travelling down the arm alongside the brachial artery and supplies no innervation to any muscle here as there are no branches above the cubital / antecubital fossa (the "elbow pit" or small triangular depression within the arm) (3, 4). The median nerve then enters the cubital fossa and passes between two heads of the pronator teres and continues to pass into the forearm between flexor digitorum profundus and flexor digitorum superficialis muscles, otherwise known as the wrist flexors.
Below shows a labelled picture for the path of the median nerve and its branches. Your practitioner learnt and practised painting with acrylics during this year's 2020 spring lockdown (figure 1):
Sensory Distribution of the Median Nerve
The median nerve supplies the sensation of the skin that naturally makes contact in a pinching motion between the thumb and fingers.
Sensory supply
for the median nerve
of the skin in the hand (6):
- The skin of the palmar and distal dorsal aspects of the lateral 3 and 1/2 (three-and-the-half) digits and adjacent palm.
- The skin of the palmar and distal dorsal aspects of the thumb and radial half of 2nd digit.
- The skin of palmar and distal dorsal aspects of the adjacent sides of 2nd–4th digits.
- The skin of the central palm.

Figure 3. Showing the sensory distribution of the median nerve.
Clinical Testing
Physical examination of the CTS involves studying the motor and sensory functions of the affected nerve in comparison to those of the ipsilateral ulnar nerve. Provocative tests to study entrapment of the median nerve.
Tinel's Sign
The Tinel’s sign is the percussion of the median nerve at the level of the carpal bones to reproduce paraesthesia in the median nerve dermatome
Phalen’s Sign
Involves holding the wrist at maximum flexion for 30 to 60 seconds to reproduce paraesthesiae in an already compromised nerve.
The severity and specificity of the clinical picture and provocative testing differ from one study to another.
However, it is considered by many that sensory symptoms, signs, and history are more important and reliable than
Phalen’s and Tinnel’s signs in the diagnosis of CTS.
Grip Strength
Motor deficit from CTS is gauged by strength assessment of the abductor pollicis brevis which is innervated by the recurrent branch of the median nerve. Clinically, patients with advanced carpal tunnel syndrome will have thenar atrophy.
Treatment For Carpal Tunnel Syndrome
- Wrist Splints: Can be worn during the day and at night. The splint can hold your wrist still whilst sleeping and can help relieve nighttime symptoms of tingling and numbness (1).
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Cortisone injection : pending on severity. Ultra sound guided cortisone injection by a qualified doctor is greatly encouraged for accuracy and efficiency.
- Surgery: Decompression surgery may be appropriate if your symptoms are severe or don't respond to other treatments (1).
Treatment Modalities Offered at the Leagrave Therapy Clinic
Electrotherapy: Ultrasound
Therapeutic ultrasound is provided at the clinic. This form of treatment is a modality that produces acoustical high-frequency vibrations (sound waves) via both thermal and non-thermal effects to the injured sight or area that is being treated (1). Deep, pulsed ultrasound over the carpal tunnel aims to reduce pain and paresthesia symptoms, sensory loss, and improves median nerve conduction and strength when compared with sham ultrasound (1). Ultrasound treatment can also provide a positive effect on sensation and patient-reported symptoms.
Posture Control and Educating 'Ideal' Spinal Alignment
It might not be commonly discussed amongst primary health setting or have enough clinical evidence to suggest that this approach may work. But, my clinical experience has taught me that neck, head, shoulder, upper back positioning and educating patients 'ideal' posture alignment and can play a big role to help upper limb pain. This approach does take patience and practice but successful results have been observed for elbow as well as wrist pain, amongst other complaints.
Massage and Sports Massage Treatment
This might be applied to structures around the affected sights and areas such as the neck, upper back, outer shoulder (e.g. deltoid muscles) as well as the hand.
Exercises:
which may involve and be applied for the wrist, neck, shoulder, elbow and posture control.
Rocktape/ Kinesiology Tape
Medical acupuncture
Gentle Spinal and Joint Manipulations
This is only performed if the techniques are redeemed appropriate. Patient informed consent must be received for each treatment modality.
References
1.) Carlson, H., Colbert, A., Frydl, J., Arnall, E., Elliot, M., Carlson, N. (2010) Current options for nonsurgical management of carpal tunnel
syndrome,
National Institute of Health, 5(1): 129–142.
2.) Ibrahim, I., Khan, W. S., Goddard, N., Smitham, P. (2012) Carpal Tunnel Syndrome: A Review of the Recent Literature, The Open Orthopedics Journal; 6: 69-76.
3.) Kanaan, N., Sawaya, R. A. (2001) Carpal Tunnel Syndrome: Modern Diagnostic and Management Techniques, British Journal of General Practice, 51:311-314.
4.) McNamara, B. (2003) Clinical Anatomy of the Median Nerve
, Anatomy Primer, ACNR, 2: 19 - 20.
5.) Neumann, D. A. (2010) Kinesiology of the Musculoskeletal System; Foundations for Rehabilitation 2nd Ed., Mosby Elsevier.
6.) Shahid, S. (2020) Median Nerve, Kenhub, online: https://www.kenhub.com/en/library/anatomy/the-median-nerve
(last visited 09/08/2020).
7.) Singh, V., Ericson, W. B. (2016) Median Nerve Entrapments, Springer International Publishing Switzerland, 369-382.
8.) Wikepedia (2020) Median Nerve, online: https://en.wikipedia.org/wiki/Median_nerve
(last visited 09/08/2020).



