Speak to a Friendly Receptionist
Whiplash Associated Disorder (WAD)
- by Joanna Blair
- •
- 07 Feb, 2024
- •
Diagnosis, Biomechanics & Physical Therapy Treatment Options.

Harold and Crewe were the first to use the term whiplash in 1928. Motor vehicle collisions (MVC) are the greatest cause for whiplash injuries and is a rather large topic within the world of physical therapies. Approximately 50% of individuals will recover following a whiplash injury within the first 3 months post injury whilst a remainder of individuals will experience mild to moderate long-term disability (9).
Whiplash-associated disorders (WAD) was defined by the Quebec task force in 1995 as ‘an acceleration–deceleration mechanism of energy transferred to the neck, it is caused by rapid hyperextension or hyeprflexion of the patient's head from sudden acceleration or deceleration (13). It may result from rear-end or side-impact motor vehicle collisions, but can also occur during driving or other mishaps.'
Despite Quebec's definition, a whiplash injury can also result from a front-end collision, however, the majority of clinical research for whiplash injuries are based around rear impact MVCs. The impact of a MVC can result in bony or soft- tissue injury (whiplash-injury). Any damage or abnormal change in soft muscular or connective tissue caused by injury are referred to as soft tissue lesions (10). A WAD is generally considered an acute soft tissue injury of the neck with symptoms such as neck pain and stiffness, shoulder weakness, dizziness, vertigo, headache, memory loss and parasthesia in the upper extremities (10).
The Classification of Whiplash
The Quebec Task Force on Whiplash Associated Disorders classifies a WAD into four grades and is based upon the severity of a person’s symptoms and signs (7):
- Grade 0: No complaints of neck pain and no physical signs.
- Grade I: Complaints of pain in the neck, stiffness or tenderness only. No physical signs.
- Grade II: Neck complaint and musculoskeletal signs including decreased range of motion and point tenderness.
- Grade III: Neck complaint, musculoskeletal signs and neurological signs including decreased or absent deep tendon reflexes, muscle weakness and sensory deficits.
- Grade IV: Neck complaint and fracture or dislocation.
Incidence
The incidence of a WAD in the UK averages to about nine per one thousand people, the highest in Europe. WADs are usually seen in rear-end, low-impact collisions in 90% of road traffic accident cases at speeds of 14 mph. Injuries occur when the trunk is forced back on the seat with hyperextension of the neck followed by a sudden forward recoil (27).
Risk
Women have thinner necks which increases their risk of whiplash. Other risk factors include individuals with short necks, car seats with a low neck rest and rear-end collisions involved with a third party heavy vehicle (27).
Car seats with an elastic back minimises the risk of neck injury after a car crash. Injury site in the majority of whiplash cases (by up to 60%) is within the zygapophysial facet joints within the neck at C2/C3 and C5/C6 levels rather than the muscles (27).

Significance

Does a Whiplash Associated Disorder Exist?
WADs have been considered to be a form of 'compensation neurosis', however, evidence suggests that whiplash injuries are real and that they are a potential cause of significant impairment (23).
A study by Aarnio et al., (2022) highlighted an important factor when it comes to WAD injuries is that; 'peripheral tissue damage can not be convincingly detected with current technologies' and the development of chronic symptoms after a whiplash injury can 'be influenced by psychological and social factors as well as changes in the central nervous system (CNS)'. They go on; 'difficulties to detect and diagnose biological contributors, together with the lack of an accepted concept for what causes the symptoms in WAD, represent considerable personal, societal, and economic problems' (1).
So, what does this mean clinically? Might it suggest that there is a lack of clinical evidence to diagnose a grade I and II (or possibly III) whiplash injury? Is the very concept of a 'WAD' for these particular grades ceasing to exist?
That last question is probably a bit melodramatic, but this post aims to answer these queries.
UK Cost
Research articles dating back to 2014 report that whiplash injuries cost the UK economy approximately £3.64 billion per year (8)! Despite the UK arguably claiming to have the safest roads in Europe, whiplash claims are also likely the highest. Fast forward on to another decade, one might assume that a few pounds can be added onto the above sum.
According to the Financial Times written in 2016, more than 800,000 small injury claims had been registered through the Ministry of Justice small claims track in 2015, of which 750,000 were estimated to be whiplash injury claims. The AA director at the time, Michael Lloyd, made the comment; “It’s little wonder that the UK is shamefully regarded as the whiplash capital of the world!” (8).
The Legal Crack Down!
To be put simply from otherwise lengthy legal jargon; the government brought forward a 'Whiplash Reform Programme' in May 2021 which was developed by the Ministry of Justice as part of the 2018 Civil Liabilities Act. Their main aim of the new whiplash reform was to reduce the number of fraudulent whiplash related claims for compensation (8).
Biomechanics of a WAD
Surprisingly, after searching around 'the biomechanics of the neck and body during whiplash injury', it appears that the medical research world has predominantly focused their attention on rear impact collisions only, despite the possibility of injury occurring during a side or front-end collision.
Although we can accept that neck injury is mostly regarded as resulting from rear end collisions, we should remind ourselves that almost one third (or approximately 27%) of all neck injuries occur from frontal impacts (16). It has been noted that there might be research papers on the biomechanics of the neck and body during the two other types of collisions.
However, none could be found in as much detail with what biomechanically happens during a rear impact collision. The focus here will be based around the biomechanics of the body during a rear impact MVC.
Biomechanics & Neck Movement During A Rear Impact Collision
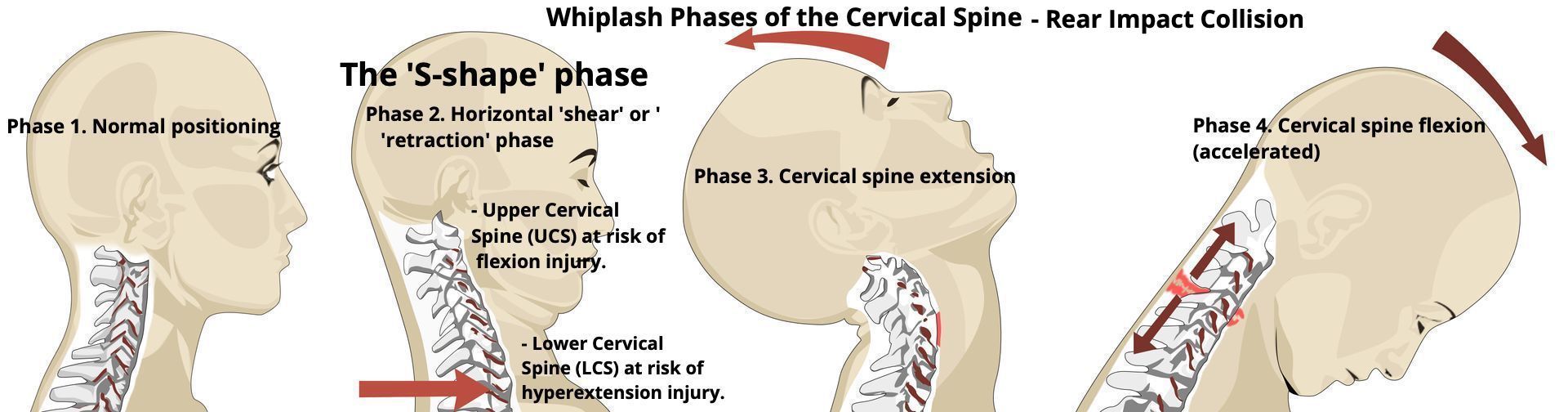
Here helps support and confirm the existence of WADs, especially for rear impact collisions. The above image demonstrates four different phases that biomechanically happen to the head and neck during such an incident. Kinematics and kinetics have been studied using crash dummies, human cadavers, human volunteers and computer models (5).
During a typical rear-end MVC, injury is caused by abnormal biomechanics of neck motion. A study by Bogduk and Yoganadan (2001) illustrated the body's response after a rear-end impact collision and showed ten different phases that the body can go through from 0 to 400 milliseconds (ms) (5). The magnitude of the cervical spine dynamics and their timing vary between subjects in different vehicles and between different subjects in the same vehicle (5).
For the sake of simplicity, it is suggested that neck movement during a rear impact collision undergoes four main stages:
I. Normal phase: The cervical spine (neck) is held in a neutral position during seated posture. Kaneoka and Ono (2002) explain how during the time period between 0-40 ms of impact, the seat already begins to press the back of an individual and the spine begins to straighten.
However, cervical motion at this stage has not yet occurred, nor is there a muscular response within the neck (15).
II. S-Shape phase: This phase occurs almost immediately following rear-impact where the neck initially undergoes a horizontal shear force. Also known as the 'retraction' phase, the neck is 'drawn back' horizontally inward to create a 'S-shaped' curvature (5, 12).
Here, simultaneous upper cervical spine (UCS) flexion occurs along with lower cervical spine (LCS) extension to force the vertebrae within the neck to create an 'S-shape' (5, 12). Neural structures in the UCS and their capsular ligaments are at risk of injury during this phase from facet joint separation and UCS flexion (5, 12, 20).
According to Panjabi et al., (2004) the potential for injury is the greatest during the s-shape phase as injurious intervertebral rotations can occur prior to when the head contacts the head rest and before cervical musculature contraction occurs to protect the spinal region (which happens later) (20). Bogduk and Yoganandan (2001) highlight how the 'sigmoid' S-shape deformation of the cervical spine occurs at between 50 to 75 ms from MVC impact.
An outcome during the S-shape whiplash phase can create changes within the cerebrospinal fluid pressure and cause a spinal ganglia injury which can potentially create pain, increased sensitivity, numbness and muscle weakness (20).
III. Cervical Spine Extension: During this phase the mandible tends to maintain its position in space whilst the upper jaw (or maxilla) lifts up off an inert mandible to open the mouth (4). The cervical spine may fully extend by approximately 200 milliseconds into a C-shape curvature post impact (5). During the extension phase, the anterior structures of the cervical vertebral column can be strained i.e. the intervertebral discs, anterior longitudinal ligaments, pre vertebral muscles and oesophagus or larynx (4). The sternocleidomastoid muscles elongate during hyperextension and posterior structures of the neck vertebrae are subject to compression such as the zygapophysial joints and the spinous processes (4).
Bogduk (1986) emphasises how the head is not thrown backwards into extension as such, rather its movement is impacted by the trunk moving forwards during this phase. The torso tends to move in a forward and upward motion upon impact whilst the head lags behind as the result of inertia (20). Thus, the torso is responsible for creating the C-shape extension curvature and not the motion of the cervical spine alone. According to Bogduk (1986), injury of the neck is at its greatest risk during the extension phase as there are no anatomical structures to stop the head from extending beyond the limit of its natural range of movement.
IV. Cervical Spine Flexion: The head achieves its maximum forward excursion by 400 ms (4). Contact of the chin with the chest limits flexion of neck movement and prevents over flexion. During this phase, the vertebrae move within the natural range of motion (4).
Medical Imaging for Whiplash
PET & CT Imaging
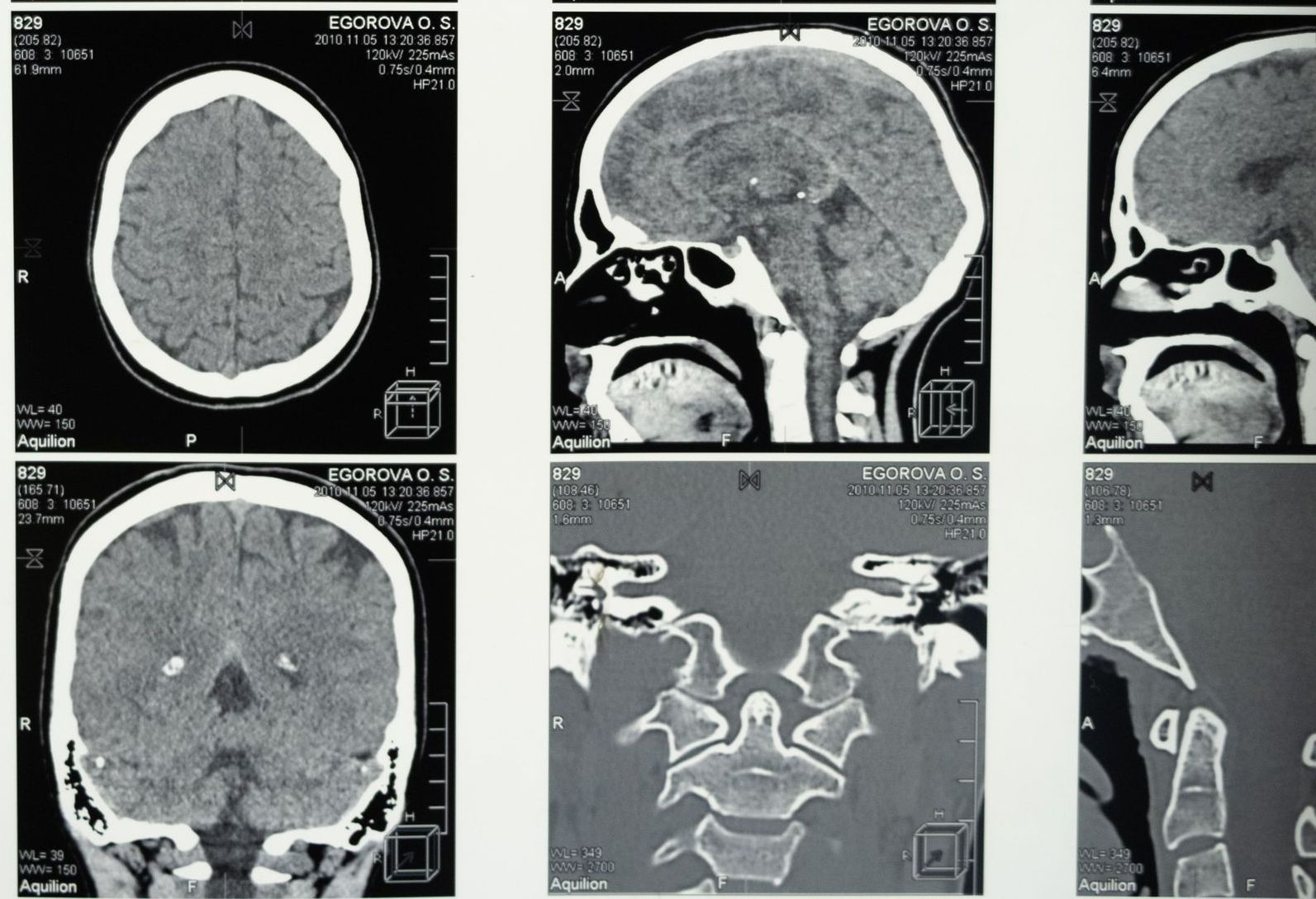
Aarnio et al., (2022) investigated whether it possible to use an objective visualisation assessment of muscular tissue inflammation in WADs using [C]-D-deprenyl positron emission tomography (PET) scan and computed tomography (CT) imaging. Whiplash injury is associated with elevated production of inflammatory mediators and PET technology has been used to detect such inflammation in tissues (1).
Their study concluded to provide evidence that tissue injury and inflammation in whiplash injury can be objectively visualised and quantified using PET and CT imaging and suggested that lesions in peripheral tissue are respnosible for the development of persistent pain and disability in whiplash injuries.
MRI Scans
Although this research study is dated back to 2006, Johansson's (2006) study is extraordinary. If litigation whiplash cases amount to the tune of over three to four billion bucks per annum, one can only ask why there are not more detailed modern research case study articles alike.
Johansson studied three injured patients post MVC who had been examined and diagnosed with no structural lesions initially. One patient, 'Patient 1', was examined via MRI scan and the second patient was examined via 'radiological examinations'. The third, 'Patient 3', underwent clinical examinations at a university hospital with no further detail provided as to what methods were used during the examination process. Two patents were initially diagnosed with 'psychogenic' or 'psychosomatic' disorders and the other signed off as 'fit to work'.
What is interesting to note is that all three patients were not diagnosed with severe lesions during their acute phases of injury post MVC after clinical examination, but were diagnosed after two to several years post MVCs. Scar tissue had been discovered in all three case studies and all underwent surgery.
In 'patient 1', scar tissue was found around the odontoid process of C2 and around C1/C2 vertebrae which affected their rotational range of movement and instability was found at C0/C1 with ligamentous injury. It was also discovered that Patients 2 and 3 had scar tissue around the odontoid process of C2 and rotational movements of their heads made either the dens or scar tissue come into contact with their spinal cord. Diagnoses originally made were reclassed as 'severe' and all patients underwent cervical surgical fixation which eradicated their extreme symptoms.
Perhaps a warning for healthcare practitioners; should patients' symptoms persist despite having had medical imaging (via MRI) during the early stages post injury of a MVC with negative findings, a request for a review via MRI, PET or CT scanning is necessary.
Treatment Options & Management

According to the NHS, symptoms of whiplash should begin to improve after a few days and significantly improve or completely diminish within one to four weeks in about 60% of cases (19). It can sometimes take a few months for the symptoms of whiplash to disappear completely and some people still have some neck pain and stiffness for a long time after the injury (19).
Wiangkham et al., (2015) concluded that conservative intervention can be effective for managing acute WAD (Type II) injuries in terms of pain reduction in the medium to long term. None invasive treatment inclusive of both physical and psychological components such as active mobilisation exercises, manual techniques, behavioural approaches and education seems to be a useful intervention (26).
Individuals at high-risk of non-recovery should receive referral to a specialist clinician with expertise in the management of WAD (31).
Cold Application Via Ice Treatment
It is advised to apply an ice pack (with a damp towel around to avoid burns) to the neck as soon as possible after the injury has occurred to help reduce inflammation, pain and swelling (19).
NB:
To avoid burns, do not apply ice directly on to skin. Wrap a damp towel around the ice pack to provide a protective barrier (19). Apply for approximately 5 - 10 minutes at a time (or to what you can tolerate within this time frame) and apply again after 20 to 30 minutes. Allow the limb to feel warm to the toucher or have a normal body temperature sensation again before reapplying.
Exercise
As NHS guidelines suggest that if pain within the neck is severe, then it is advised to rest the neck for 24 to 48 hours until the pain eases (19). Exercising the neck gently can help prevent the neck joints from becoming too stiff. Movements need to be performed very slowly and to the range that can be achieved within each direction to gradually increase range of movement.
Certain exercises, such as strengthening exercises can slow recovery when compared with simple mobilisation exercises. Remaining active is critical but attention is needed to ensure exercise programs are not too aggressive as more aggressive programs may reaggravate healing tissues (28).
Painkillers
The NHS advises that painkillers, such as paracetamol, can help ease the pain caused by whiplash. Taking painkillers regularly rather than only when the pain is severe, please read the instructions carefully and do not exceed the recommended dose (19).
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help reduce inflammation (swelling) within the neck, check first for which medications can be medically taken. If usual painkillers are not enough, the doctor can advise and may prescribe a stronger painkiller, such as codeine (19).
Posture
Maintaining a good, upright posture whilst sitting, standing and walking can help prevent the pain and stiffness within neck getting worse (19). Supporting the head with a firm pillow will help maintain a good sleeping posture (19).
Massage
From reading the research, massage therapists need to be experienced in this field with knowing where and when it is appropriate to apply soft tissue massage. For instance, it is not appropriate to apply massage to individuals with a type III or IV whiplash injury and instead need to be referred to either their general practitioner or emergency A & E department.
Research suggests that the application to WAD Type II injuries can reproduce symptoms when applied to the upper cervical spine muscles or even make symptoms worse (21).
A study by Griffin et al., (2019) concluded that there was a higher incidence of recovery at 3-months post injury in individuals who had received 'non-recommended (passive) treatments' mainly including massage and a fewer percentage receiving either chiropractic and osteopathy treatment. According to this study, 'evidence-based care (EBC)' i.e. with use of WAD specialists, including rehabilitation physicians, specialist physiotherapists, psychologists and occupational physicians was not significantly associated with recovery for WAD at 3 months post injury (11).
Exercise
Conlin et al., (2005) concluded that exercise alone does not improve ROM in patients with acute WAD and that gentle hands on mobilisation techniques are recommended for the treatment of pain and compromised cervical range of motion in the acute WAD patient.
From the literature read, phsyiotherapy can help provided that the correct exercises are prescribed. Strengthening or prescribing wrong exercises, especially during the early stages of recovery can make symptoms worse.
Osteopathy
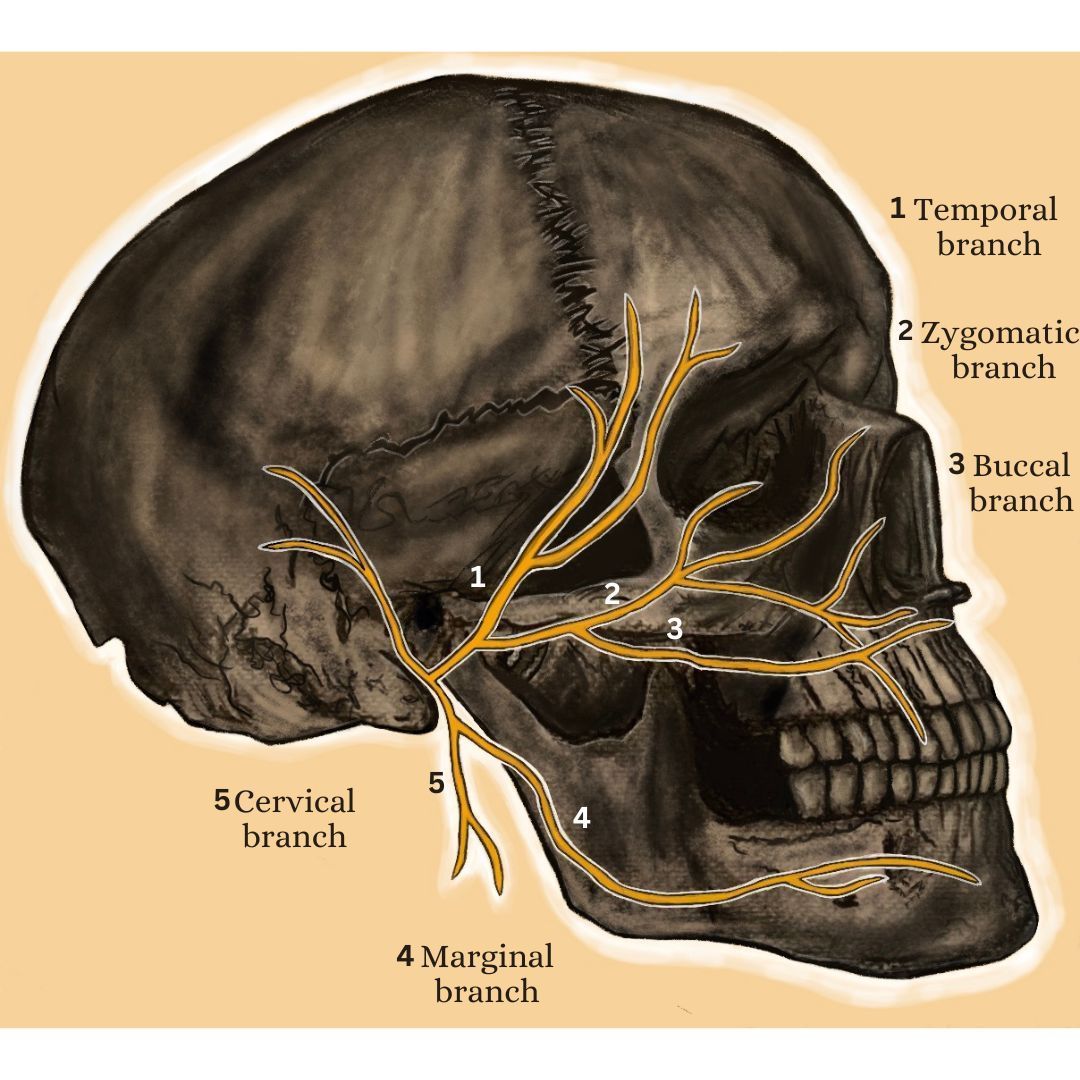
A study by Parravicini and Ghiringhelli (2021)found that cranial osteopathy and soft tissue trigger point massage application to specific regions of the cranium such as the occiput, mastoid process and the temporal bone can help alleviate symptoms. Gentle joint mobilisation or passive joint movement techniques by the therapist's hands can help restore physiological cervical spine active range of movement (18). Spinal manipulations would be a contraindication and not performed especially during the acute (up to 4 weeks) or subacute phases (4 to 12 weeks).
Long-term problems arising from whiplash
In a small number of cases, the pain caused by whiplash can become chronic (long-term). In severe whiplash cases, the pain can last for more than six months before it disappears (19).
References
1. Aarnioa, M., Fredrikson, M., Lampa, E., So ̈rensene, J., Gordha, T., Linnman, C. (2022)Whiplash injuries associated with experienced pain and disability can be visualized with [11C]-D-deprenyl positron emission tomography and computed tomography, Pain, 163; 3: 489-495.
2. Alicia, T., Kapur, S., Mutagi, H. (2014) Whiplash Injury, Continuing Education in Anaesthesia, Critical Care & Pain, 14; 4: 167-170.
3. Bannister, G., Amirfeyz, R., Kelley, S., Gargan, M., Whiplash Injury; Review Article, The Journal of Bone and Joint Surgery, 91; 7: 845-850.
4. Bogduk (1986) The Anatomy and Patholophysiology of Whiplash: Review Paper, Clinical Biomechanics, 1:92-101.
5. Bogduk, N., Yoganandan, N. (2001) Biomechanics of the Cervical Spine Part 3: Minor Injuries [Review Paper], Clinical Biomechanics, 16:267-275.
6. Conlin A, Bhogal S, Sequeira K, Teasell R. (2005) Treatment of whiplash associated disorders. Part I: Non-invasive interventions. Pain Res Manage, 10 (1): 21-32.
7. Ferrari, R. (2002) Prevention of Chronic Pain After Whiplash, Emerg Med J, 19: 525-530.
8. Financial Times (2016)Whiplash Injury Payouts Face Government Crack Down https://www.ft.com/content/9e155cb6-ac18-11e6-9cb3-bb8207902122 [online].
9. Ghoryab, J. H. (2021) The nosological classification of whiplash-associated disorder: a narrative review, The Journal of the Canadian Chiropractic Association, 65; 1: 76-93.
10. García, D. V., Doorduin, J., Willemsen, A, T. M., Dierckx, R. A. J. O., Otte, A. (2016) Altered Regional Cerebral Blood Flow in Chronic Whiplash Associated Disorders, 10: 249-257.
11. Griffen, A., Jagnoor, J., Arora, M., Cameron, I. D., Kifleym A., Sterling, M.,Kenardy, J., Rebbek, T. (2019) Evidence-based care in high- and low-risk Groups following whiplash injury: a multi-centre inception cohort study, BMC Health Services Research, 19: 806.
12. Hai-bin, C., Yang, K. H., Zheng-gun, W. (2009) Biomechanics of Whiplash Injury, Chinese Journal of Traumatology, 12; 5: 305-314.
13. Ivancic, P. C., Ito, S., Tominaga, Y., Rubin, W., Coe, M. P., Ndu, A. B., Carlson, E. J., Panjabi, M. M. (2008) Whiplash Causes Increased Laxity of Cervical Capsular Ligament, Clinical Biomechanics, 23: 159-165.
14. Johansson, B. H. (2006) Whiplash Injuries Can be Visible By Functional Magnetic Resonance Imaging: Case Report, Pain Res Manage, 11; 3: 197-199.
15. Kaneoka, K., Ono, K., Inami, S. et al. (2002) The Human Cervical Spine Motion During Rear Impact Collisions: A Proposed Cervical Facet Injury During Whiplash Trauma, J. Whiplash Related Disord, 1; 1: 85-97.
16. Kullgren, A., Krafft, M., Nygren, A., Tingvall, C. G. (2000) Neck injuries in frontal impacts: Influence of crash pulse characteristics on injury risk, Accident Analysis & Prevention, 32; 2: 197-205.
17. Lee, S-H., Park, S-Y., Heo, I., Hwang, E-H., Shin, B-C., Hwang, M-S. (2023) Efficacy of acupuncture for whiplash injury: a systematic review and meta- analysis, BMJ Open, 14: 1-10.
18. McClune, T., Burton, A. K., Waddell, G. (2002) Whiplash associated disorders: a review of the literature to guide patient information and advice, Emerg Med J., 19: 499-506.
19. NHS Royal Berkshire: NHS Foundation Trust, Neck Injury (Whiplash / Neck Sprain)
20. Panjabi, M. M., Pearson, A. M., Ito, S., Ivancic, P. C., Wang, J-L. (2004) Cervical Spine Curvature During Simulated Whiplash, Clinical Biomechanics, 19: 1-9.
21. Parravicini, G., Ghiringhelli, M. (2021) Osteopathic Cranial Manipulation for a Patient With Whiplash-Associated Disorder: A Case Report, J Chiropractor Med., 20; 3: 163-169.
22. Peolsson, A., Hermansen, A., Peterson, G., Strid, E. N. (2021) Return to work a bumpy road: a qualitative study on experiences of work ability and work situation in individuals with chronic whiplash-associated disorders, BMC Public Health, 21; 785: 1-11.
23. Pho, C., Godges, J. (2004) Management of Whiplash-Associated Disorder Addressing Thoracic and Cervical Spine Impairments: A Case Report, Journal of Orthopaedic & Sports Physical Therapy, 34;9: 511-523.
24. Ronnen, H. R., Korte, P. J. de., Brink, P. R., Bijl, H. J. van der, Tonino, A. J., Franke, C. L. (1996) Acute whiplash injury: is there a role for MR imaging?- a prospective study of 100 patients, 201, 1.
25. Schofferman, Bogduk, N., J., Slosar, J. (2015) Chronic Whiplash and Whiplash-Associated Disorders: An Evidence- Based Approach, Journal of the American Academy of Orthopaedic Surgeons: 596-606.
26. Sterling, M. (2014) Physiotherapy management of whiplash-associated disorders (WAD), Journal of Physiotherapy, 60: 5-12. *
27. Sterling, M., Vincenzino, B., Souvlis, T., Connelly, L.B. (2015). Dry-needling and exercise for chronic whiplash-associated disorders: a randomized single-blind placebo-controlled trial. Pain, 156,
635 – 643.
28. Tameem, A., Kapur, S., Mutagi, H. (2013) Whiplash Injury, Continuing Education in Anasethesia, Critical Care and Pain: 1-4.
29. Teasell, R. W., McClure, J. A., Walton, D., Pretty, J., Salter, K., Meyer, M., Sequeira, K., Death, B. (2010) A Research Synthesis of Therapeutic Interventions for Whiplash-Associated Disorder (WAD):Part 2 – interventions for acute WAD, Pain Res Manage, 15; 5: 295-304.
30. Watson, E. D., Coopoo, Y. (2010) Popular physical therapy modalities in the management of whiplash-associated disorders, SAJSM, 22; 4: 95-98.
31. Wiangkham, T., Duda, J., Haque, S., Madi, M., Rushton, A. (2015) The effectiveness of conservative management for acute whiplash associated disorder (WAD) II: a systematic review and meta-analysis of randomised controlled trials. PLoS One.; 10.