Shoulder Pain & Subacromial Impingement Syndrome (SAIS)
- by Joanna Blair
- •
- 27 Sept, 2018
- •
Impingement Can be Classified into 4 Types:
1.)
Subacromial impingement syndrome (external
impingement).
2.) Subcoracoid impingement.
3.) Posterosuperior (inner) impingement.
4.) Anterosuperior (inner) impingement.
This blog post will be focusing on subacromial impingement syndrome (SAIS).
How Common Is SAIS?
Shoulder impingement syndrome is the most commonly diagnosed
shoulder disorder and more often present in dominant than non dominant shoulders which typically develops over a period of weeks to months (4, 5).
According to Michner et al.,
(2003),
the incidence of (SAIS) of all shoulder pain complaints account for
approximately 44-65% and as a consequence cause a functional loss and
disability within the joint and make normal daily activities such as combing one's hair or reaching up to cupboards painful.
Commonly found in people:
· Over the age of 40.
· Suffer from persistent pain.
· Idiopathic cause without any known preceeding trauma.
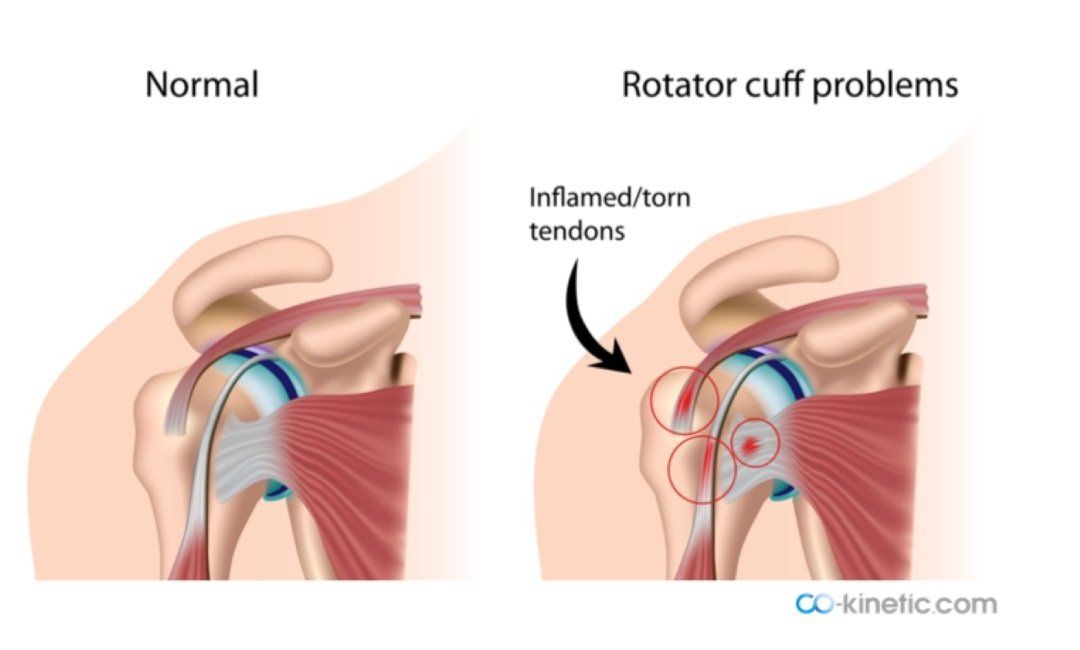
The most common clinical diagnoses amongst shoulder complaints are rotator cuff muscle defects i.e. tears (85%) and/ or shoulder impingement syndrome (74%) (2). Changes in scapular kinematics (mechanics) that cause subjects to accumulate SAIS generally have decreased scapular posterior tilting, reduced upward rotation and increased internal rotation of the GHJ (5). Weak scapular musculature, fatigued infraspinatus and teres minor muscles are also associated along with changes of thoracic and cervical spine posture (5).
The prevalence of rotator cuff muscle defects tends to increase with age with a considerable proportion
of individuals being over the age of sixty years (2). Garving et al.,
(2017) reports that statistically, 30% of individuals over the age of 70 have a total defect but 75% of cases are asymptomatic (report no symptoms). Latest talks by orthopedic surgeons that I have recently attended explain the requirement of manual rehabilitation treatment for the problem rather than the use of operative intervention for this age group.
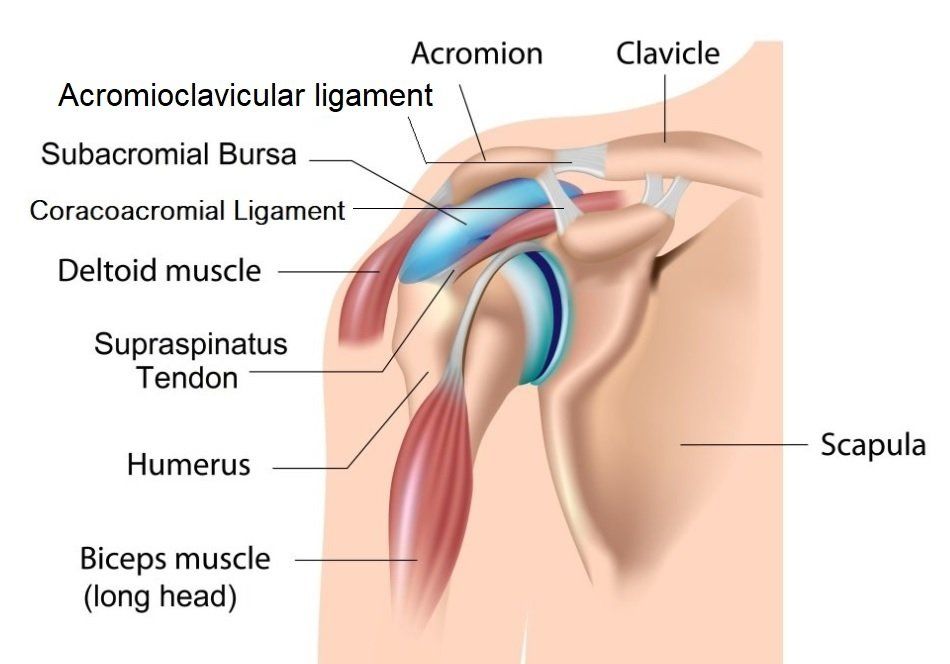
Anatomy of the Subacromial Space
- Humeral head inferiorly.
- The under surface of the anterior third of the acromion.
- coracoacromial ligament.
- acromioclavicular joint superiorly.
- The supraspinatus tendon.
- Subacromial bursa.
- Long head of biceps brachii tendon.
- Capsule of shoulder joint.
Primary and Secondary Impingement
Subacromial
impingement has both primary and secondary forms.
Primary Impingement:
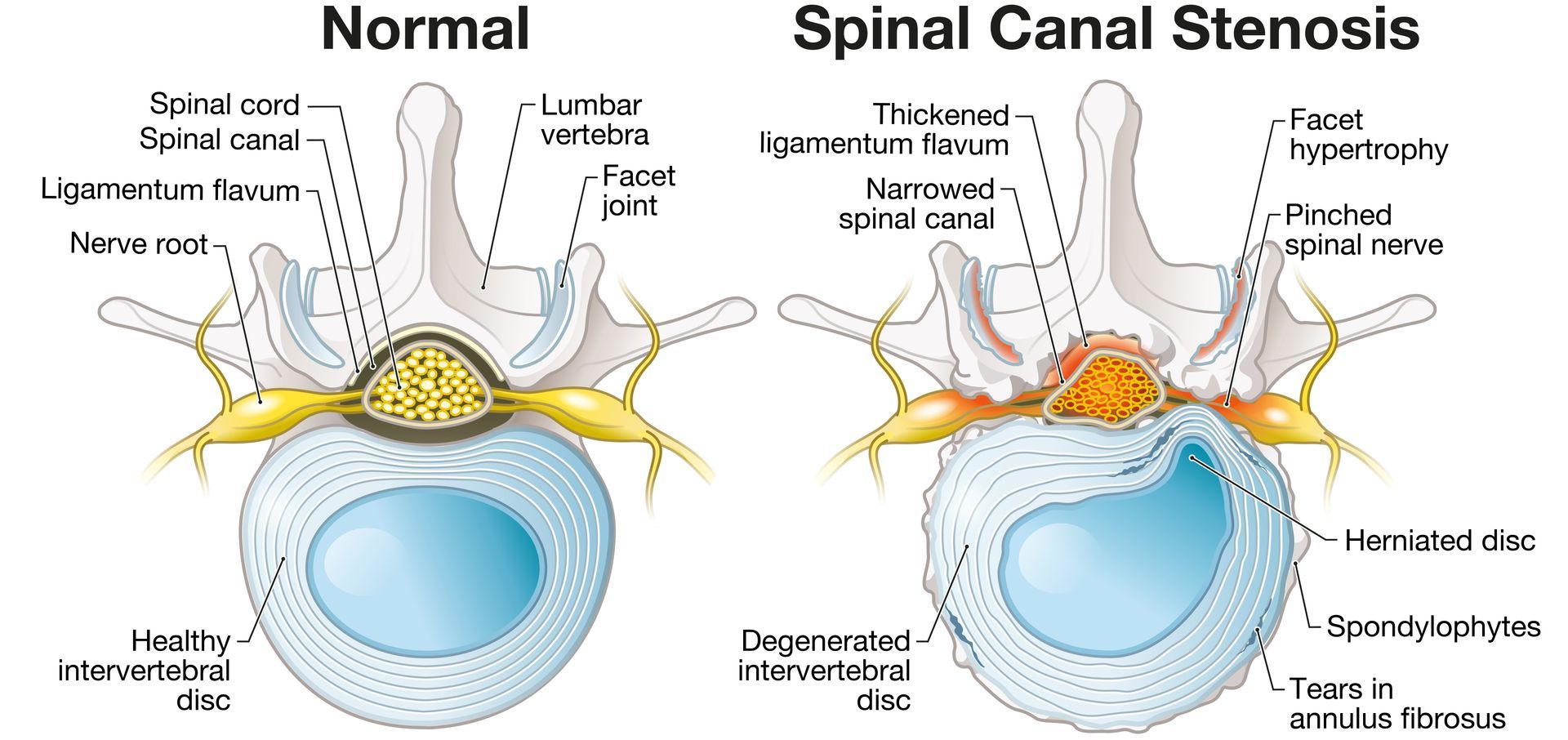
Primary impingement has been described by Neer as ‘impingement of the rotator
cuff beneath the coracoacromial arch’ and is due to structural changes
which cause the subacromial space to narrow. This
might be caused via bony narrowing of the joint or increased volume of the subacromial soft tissues due to
e.g. subacromial bursitis or calcific tendonitis (figure 2) (2).
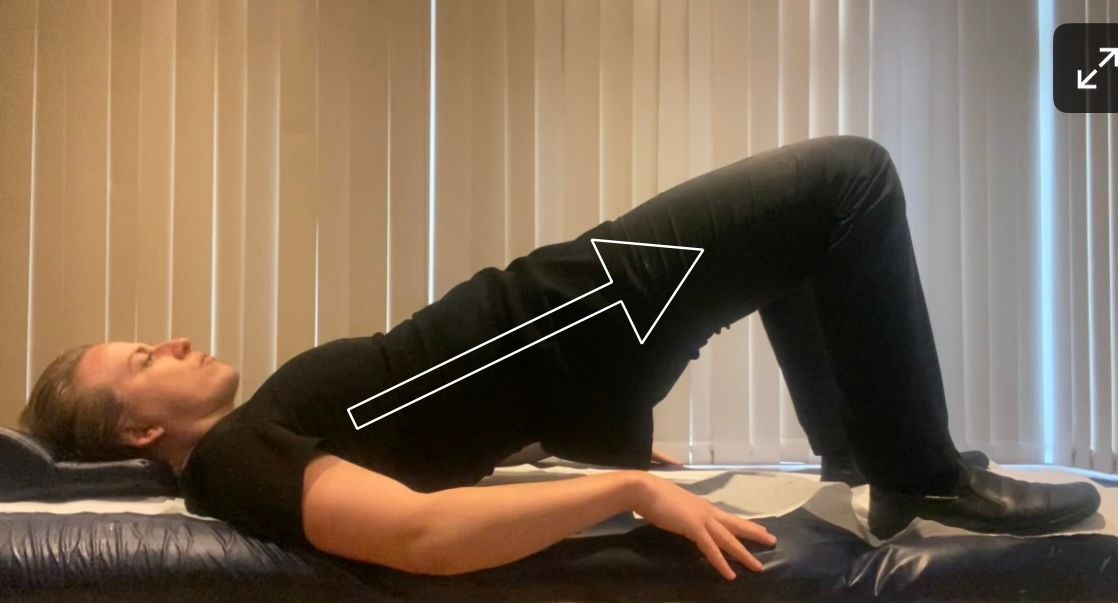
Primary impingement may result from subacromial crowding, posterior capsular tightness or excessive superior migration of the humeral head due to weakness of the humeral head muscle depressors.
Secondary Impingement:
According to Garving et al., (2017), secondary impingement is a decrease of the subacromial space due to scapulothoracic instability or a functional disturbance of the GHJ causing the centering of the humeral head with relation to the glenoid fossa to not be in the ideal position. It can be caused by a muscular imbalance leading to soft tissue entrapment or triggered by weakness of the rotator cuff mechanism and the biceps tendon (3). The end result of both syndromes is rotator cuff tendon inflammation and potential rupture.
Extrinsic & Intrinsic Factors
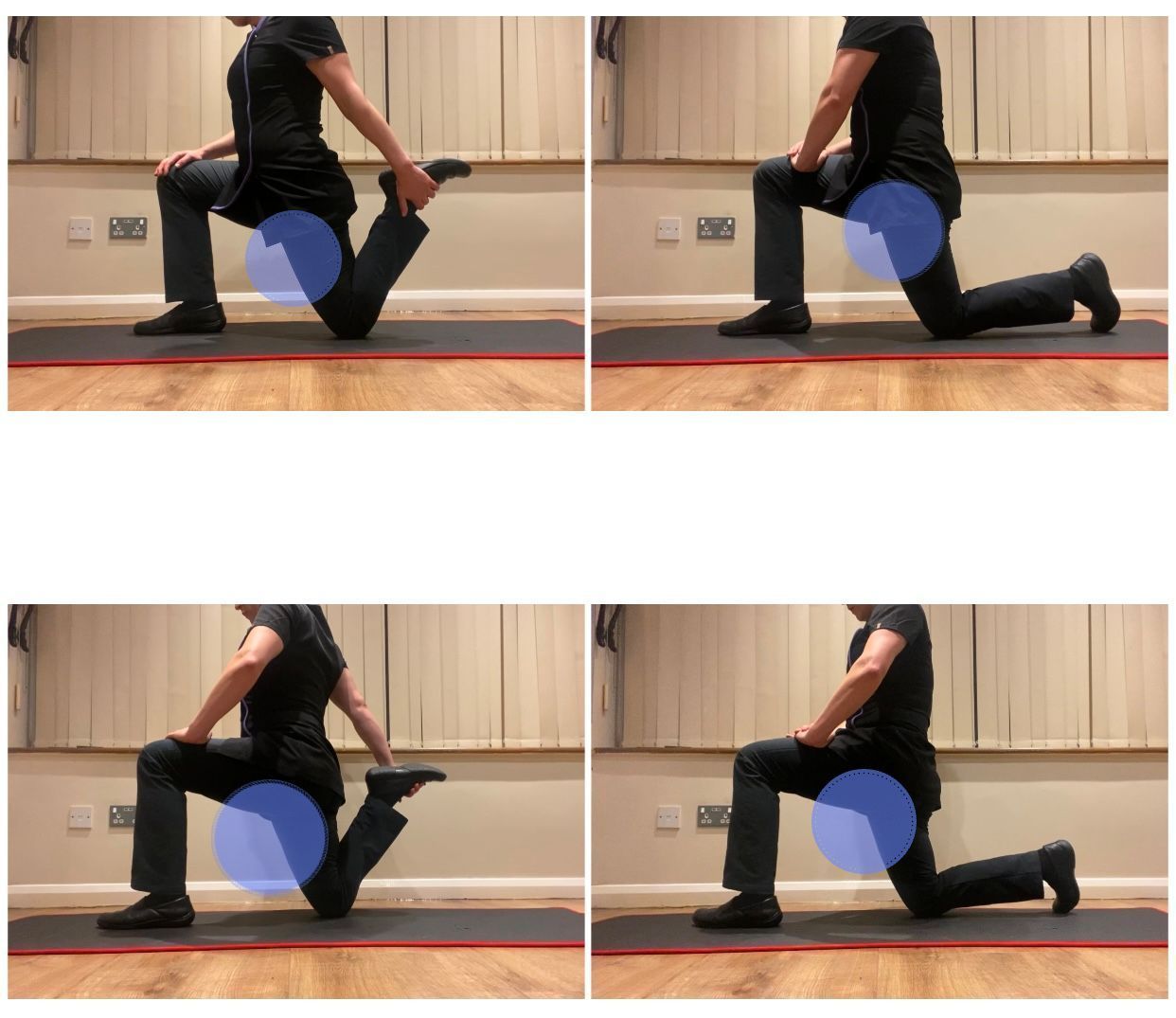
Mackenzie et al., (2015) describe how pathological factors that may contribute to impingement syndrome can be divided into extrinsic and intrinsic factors.
Extrinsic factors include the compression of rotator cuff tendons caused by alignment factors, anatomic factors, scapular kinematic factors, muscle imbalance, sport specific and ergonomic factors.
Intrinsic factors that may contribute to rotator cuff tendon degeneration due to shear forces and overload, mechanical properties, morphology and vascularity within the tendon (4).
Further Anatomical Factors
2. Thickening of the coracoacromial ligament (figure 1) (5).
3. Reduced force output and muscle performance of the trapezius and serratus anterior muscles (5).
4. Weakness of rotator cuff musculature (5).

What Activities Commonly Make SAIS Worse?
SAIS is typically made worse by (2):
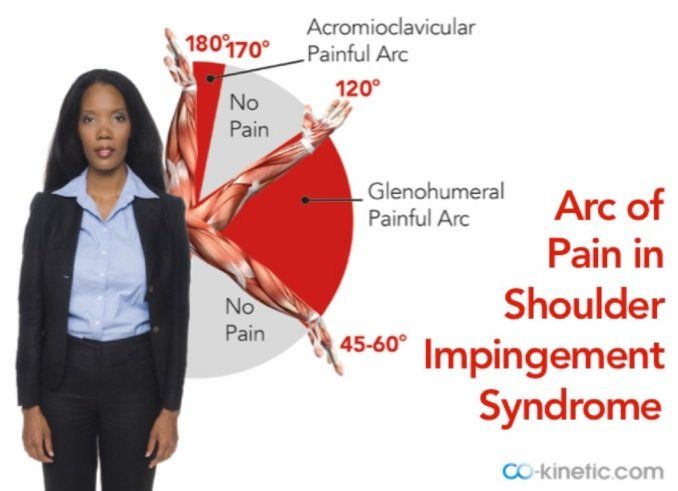
1.) Elevating the arm between 70 and 120 degrees, known as “painful arc” (Figure 3).
2.) Forced movement above the head.
3.) Lying on the affected side.
References
3. Kamkar, A., Irrgang, J. J., Whitney, S. L. (1993) Nonoperative Management of Secondary Shoulder Impingement Syndrome, Cinical Commentary, JOSPT,17; 5: 212-224.
4. McKenzie, T. A., Herrington, L., Horsley, I., Cools, A. (2015) An Evidence-Based Review of Current Perceptions with Regard to the Subacromial Space in Shoulder Impingement Syndromes: is it Important and What Influences it? Clin Biomech, 30; (7): 641-8.